Wazzup Pilipinas!?
A Revolutionary Discovery in the Fight Against the Philippines' Deadliest Women's Cancer
In the sterile quiet of a University of the Philippines laboratory, Dr. Regina Joyce Ferrer peers into a microscope at what might look like tiny, insignificant clusters of cells floating in a petri dish. But these breast cancer organoids—miniature replicas of human tumors grown in controlled conditions—hold secrets that could transform how doctors treat one of the Philippines' most devastating diseases.
These laboratory-grown tissues have just helped unlock a medical breakthrough that could save thousands of Filipino women's lives.
The Silent Killer's Staggering Toll
The statistics paint a sobering picture of breast cancer's grip on Filipino women. In 2022 alone, over 33,000 new cases emerged across the archipelago—equivalent to roughly 90 women receiving this life-altering diagnosis every single day. More heartbreaking still, the disease claimed over 11,000 lives that same year, making it the second-leading cause of cancer deaths in the Philippines, trailing only lung cancer.
But behind these numbers lies an even more sinister reality: many of these deaths could potentially be prevented if doctors had better tools to predict which cancers would turn aggressive and spread to other organs—a deadly process called metastasis.
The Race Against an Invisible Enemy
When breast cancer decides to become a killer, it doesn't announce its intentions. Instead, it begins a stealthy invasion, sending rouge cells through the body's lymphatic system and blood vessels in a process called lymphovascular invasion, or LVI. This biological betrayal serves as the cancer's highway system, allowing malignant cells to establish deadly colonies in distant organs.
For doctors, detecting LVI has been like trying to spot a burglar after the house has already been robbed. Current methods require surgical removal of the tumor and surrounding tissue—meaning physicians can only confirm this critical warning sign after invasive procedures have already taken place.
But what if they could identify this threat much earlier, before the first incision is ever made?
A Mathematical Crystal Ball
Dr. Michael Velarde and his team at the University of the Philippines Diliman College of Science have developed what amounts to a mathematical crystal ball—a predictive model that can detect lymphovascular invasion in breast cancer patients before they even undergo surgery.
"If we can detect LVI earlier, doctors could personalize patient treatment and improve their outcomes," explains Dr. Velarde, the study's lead researcher. "This could help avoid ineffective treatments and focus on strategies that work better for aggressive breast cancer."
The implications are staggering. Instead of waiting to discover whether a patient's cancer has begun its deadly migration, doctors could know from the very beginning which patients need the most aggressive treatment protocols.
Unraveling the Mystery of Drug Resistance
The research team's investigation began with a troubling observation from clinical data involving 625 breast cancer patients at Philippine General Hospital. They noticed a disturbing pattern: patients with lymphovascular invasion consistently responded poorly to standard anticancer drugs like doxorubicin and anthracyclines.
This finding led them down a scientific rabbit hole that would ultimately crack open one of breast cancer treatment's most vexing puzzles—why some tumors simply shrug off chemotherapy that should, by all medical logic, destroy them.
Working with tumor samples cultivated into organoids—essentially growing miniature versions of patients' cancers in laboratory conditions—the researchers confirmed their suspicions. LVI-positive organoids demonstrated remarkable resistance to the very drugs designed to eliminate them.
The Genetic Saboteurs
The answer lay hidden in the patients' genetic code. Dr. Velarde's team discovered that certain genes, particularly the UGT1 and CYP gene families, were significantly more active in patients with lymphovascular invasion. These genes function like microscopic recycling plants, breaking down anticancer drugs before they can do their job.
In patients with high activity of these genetic saboteurs, chemotherapy drugs are metabolized and eliminated so rapidly that they barely have time to attack the tumor. It's like trying to fill a bucket with a massive hole in the bottom—no matter how much you pour in, it disappears before it can accumulate enough to make a difference.
A 92% Accurate Prediction
Armed with this knowledge, the research team constructed a regression model that analyzes the expression patterns of these drug-resistance genes. The results were remarkable: their model correctly predicted LVI status 92% of the time, using only biopsy samples taken before any surgical intervention.
This level of accuracy represents a quantum leap in predictive oncology. For the first time, Filipino doctors could potentially know, with near-certainty, which of their breast cancer patients are harboring tumors primed for aggressive spread and drug resistance.
Hope with Realistic Expectations
Despite the breakthrough's promise, Dr. Velarde maintains scientific caution about the model's current limitations. "The model is still in its early stages of development and is not yet ready to replace current methods for diagnosing LVI," he emphasizes. "More validation studies are needed before this can be used in clinics."
The research team plans to expand their validation efforts by testing the gene signatures of larger groups of Filipino breast cancer patients. They're also investigating how UGT1 and CYP genes specifically contribute to lymphovascular invasion, with hopes of identifying drug combinations that could overcome this resistance in LVI-positive patients.
A Uniquely Filipino Solution
Perhaps most importantly, this breakthrough was designed with Filipino patients in mind. "Our approach can be implemented in the Philippines using locally available genomic technologies, making earlier detection and tailored treatment more accessible to Filipino patients," Dr. Velarde notes.
This represents more than just scientific advancement—it's a homegrown solution to a distinctly Filipino health crisis, developed by Filipino scientists for Filipino patients using technologies already available in Philippine hospitals.
The Road Ahead
The ultimate goal, according to Dr. Velarde, is both ambitious and deeply personal: "Our goal is to develop a practical test that can be used in Philippine hospitals to guide doctors in choosing the best treatment for each patient."
Imagine a future where every Filipino woman diagnosed with breast cancer receives a treatment plan tailored specifically to her tumor's genetic fingerprint. Where doctors know from day one whether standard chemotherapy will work, or whether more aggressive interventions are needed. Where the difference between life and death might come down to a genetic test that costs a fraction of current treatment protocols.
Beyond the Laboratory
While the organoids in Dr. Ferrer's laboratory continue to reveal their secrets, the real impact of this research will be measured not in published papers or scientific accolades, but in lives saved. Every percentage point improvement in treatment effectiveness translates to hundreds of Filipino mothers, daughters, sisters, and wives who might have a fighting chance against this disease.
The work represents a powerful example of how locally-developed research can address locally-specific health challenges. Rather than waiting for solutions developed in distant laboratories for different populations, Filipino scientists are pioneering approaches designed specifically for the genetic and clinical realities of Filipino patients.
A New Chapter in Cancer Care
As Dr. Velarde and his team prepare for the next phase of their validation studies, they carry with them the weight of tremendous possibility. Their mathematical model might seem abstract, but its potential impact is viscerally real—written in the stories of women who might live to see their children graduate, celebrate grandchildren's births, or simply enjoy another sunrise because their doctors had better tools to fight their disease.
The fight against breast cancer in the Philippines has entered a new chapter, one where prediction might prove more powerful than reaction, where personalized medicine becomes accessible rather than aspirational, and where Filipino innovation leads the charge against one of the nation's deadliest foes.
In laboratories across the University of the Philippines, the future of breast cancer treatment is taking shape, one organoid at a time. And for the 90 Filipino women who will receive their diagnosis today, that future can't come soon enough.




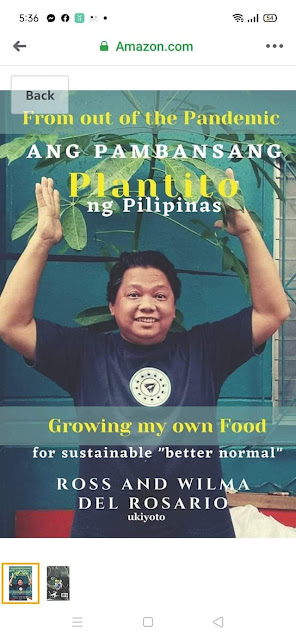
















 Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.
Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.






.jpg)





Post a Comment