Wazzup Pilipinas!?
In a world where invisible enemies evolve faster than the tools designed to fight them, a recent report from the World Organisation for Animal Health (WOAH) delivers a message both hopeful and cautionary. Between 2020 and 2022, antimicrobial use in 71% of the global animal biomass fell by 5%. It’s a milestone worth celebrating—but far from a final victory.
Beneath the surface of this achievement lies a critical warning: in 2022 alone, 8% of antimicrobials administered to animals were categorized as high-priority critically important medicines for human health. These are the last lines of defense in human medicine—the drugs we turn to when all others fail. Their use in animals, especially when unnecessary or excessive, threatens to accelerate antimicrobial resistance (AMR), turning minor infections into potential death sentences for both people and animals.
Nowhere is this global issue more starkly framed than in Africa—where challenges in surveillance, regulation, and resources intersect with immense opportunity for leadership in sustainable solutions.
Africa’s Opportunity and Burden in the Antimicrobial Era
Africa is no stranger to the silent creep of antimicrobial resistance. With rising demands for animal protein, growing agricultural industries, and limited regulatory frameworks in some regions, the continent stands on a delicate precipice.
But the story is far from bleak. The WOAH report reveals that Africa is slowly but surely stepping up.
1. Surveillance: Progress Amidst Patchwork
Surveillance is the foundation of informed action. Across the continent, nations are increasingly participating in global data-sharing initiatives such as ANIMUSE, the WHO’s global database for monitoring antimicrobial use in animals. These systems are crucial for identifying trends, hotspots, and potential risks.
Yet gaps remain. Many African nations still face infrastructural and technical hurdles in gathering, verifying, and reporting antimicrobial data. Without robust national surveillance networks, blind spots in AMR development will continue to persist—posing risks not just locally, but globally.
2. Responsible Use: Culture Versus Crisis
In some African regions, antimicrobials—especially antibiotics—are still used indiscriminately, not just to treat disease, but as growth promoters in livestock production. This practice, though cost-effective in the short term, fast-tracks the development of resistance.
What is urgently needed is stronger regulation and enforcement, as well as a shift in veterinary practice norms. Educational outreach to farmers, tighter import controls, and capacity-building for veterinary professionals are all critical pieces of this puzzle.
3. Embracing the One Health Approach
The key to defeating AMR doesn’t lie in a single lab or clinic—it lies in embracing the One Health concept: the recognition that human, animal, and environmental health are inseparably linked.
Institutions like CIRAD and the Pasteur Institute are leading the way, fostering multidisciplinary collaboration to develop AMR solutions that span species and ecosystems. Africa, with its unique biodiversity and interconnected communities, is well-positioned to become a global model for One Health implementation—if the political will and financial support are there.
4. Prevention, Not Just Cure: Investing in Vaccines and Welfare
Perhaps the most powerful weapon against antimicrobial overuse is not a better antibiotic—it’s a healthier animal. African nations must increase investments in animal vaccination, biosecurity, and improved living conditions for livestock.
Developing and distributing vaccines that are adapted to Africa’s diverse environments could drastically reduce the need for antimicrobials. But such innovation requires funding, research capacity, and regional collaboration—all of which are currently underdeveloped.
A Global Threat, A Continental Responsibility
Africa’s role in the global AMR battle cannot be overstated. While the WOAH report shows global momentum, the stakes for Africa remain particularly high.
In a world more interconnected than ever, drug-resistant pathogens know no borders. A resistant strain emerging from a poorly regulated farm in one country can reach hospitals on another continent in days. Thus, Africa’s success in this fight is the world’s success.
The Road Ahead: From Promise to Protection
The 5% reduction in antimicrobial use offers hope. But that hope is fragile. The continued misuse of high-priority medicines in animals represents a dangerous loophole that could undermine decades of medical progress.
Africa now stands at a pivotal moment: equipped with the knowledge of what must be done, supported by growing international frameworks, and driven by the urgency of protecting future generations.
To truly win this fight, surveillance must be strengthened, regulations must be enforced, antibiotic alternatives must be embraced, and the One Health approach must be institutionalized.
The clock is ticking—but with bold action and global solidarity, Africa can lead the way in securing a world where antibiotics still work, for humans and animals alike.






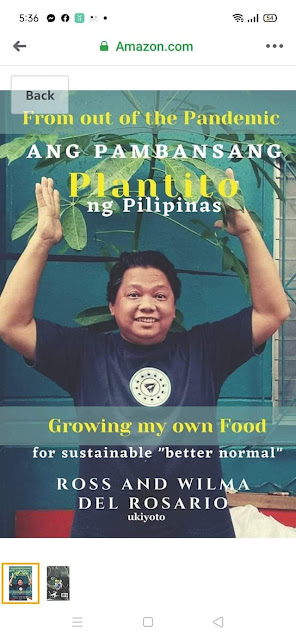
















 Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.
Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.








.jpg)


