Wazzup Pilipinas!?
Milk has long stood as a universal symbol of nourishment, sharing, and community. From rural homesteads to bustling city markets, it graces our tables as both a childhood staple and a culinary foundation. But behind this comforting glass lies an overlooked truth—one that now demands our collective attention.
As we raise our glasses in celebration of this life-sustaining product, we must also confront a dangerous and often invisible threat: veterinary drug residues in milk. This issue, particularly acute in several regions of Africa, is more than a food safety concern—it is a ticking time bomb for global health.
The Silent Saboteur: Antibiotic Residues in Dairy
The problem originates in a critical lapse: the non-compliance with veterinary drug withdrawal periods—the mandated time between administering medication to livestock and using their milk for human consumption. When these guidelines are ignored, residual drugs can pass directly into the milk supply.
The consequences are deeply troubling:
Human Health at Risk: Consumption of milk tainted with antibiotics can provoke allergic reactions in vulnerable individuals. More dangerously, it contributes to antimicrobial resistance (AMR)—one of the gravest health threats of our time. As bacteria become resistant to commonly used medications, once-curable infections become deadly. AMR is already claiming hundreds of thousands of lives annually and is projected to surpass cancer as a leading cause of death by 2050 if unchecked.
Broken Food Systems: Beyond health, there are serious technological implications. Antibiotic residues interfere with the fermentation processes crucial to making cheese, yogurt, and other dairy products. The result? Spoiled batches, financial loss, and food insecurity.
Economic Fallout and Trade Barriers: In the global market, food safety is non-negotiable. Milk that fails residue tests can be rejected, harming not just individual farmers but entire economies dependent on dairy exports.
A Call to Conscience: Reimagining Dairy with Dignity
This crisis isn’t unsolvable—but it demands urgent, united action. A sustainable dairy future hinges on shared responsibility. Every actor in the milk value chain must rise to the challenge:
Farmers must receive training and support to understand drug withdrawal periods and invest in good animal husbandry practices.
Veterinarians must lead with vigilance, ensuring prescriptions are administered appropriately and withdrawal times are clearly communicated.
Regulators and health authorities must establish rigorous monitoring systems and enforce compliance, while educating the public.
Consumers, too, have power—by demanding transparency, supporting responsible producers, and raising their voices for better standards.
Milk as a Mirror of Our Morality
We cannot continue to toast to the bounty of milk while ignoring the silent erosion of its safety. It is time to align our reverence for this nourishing liquid with our responsibility to ensure its integrity—from farm to table.
Today, as we honor milk as a staple of our diets and a symbol of community strength, let us also reaffirm our commitment to responsible dairy production. Let every glass reflect not just nutrition, but excellence, ethics, and care.
We have the tools. We have the knowledge. What we need now is the will to act.
Let us make milk not just a tradition—but a testament to sustainable health for generations to come.






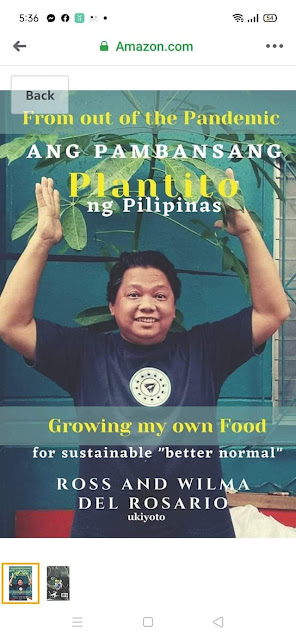
















 Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.
Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.






.jpg)




