Wazzup Pilipinas!?
She never saw it coming.
But for millions of Indian women and children, a silent predator is eroding health from within. It doesn’t announce itself. It doesn’t leave fingerprints. It drifts in on the wind. It is PM₂.₅, fine particulate pollution — and over long periods, it is being linked to a cascade of illnesses: hypertension, diabetes, chronic lung disease, anemia, low birth weight, respiratory infections in kids.
Now, armed with a powerful interactive dashboard, researchers are connecting the dots — mapping how decades of exposure to dirty air are manifesting in bodies, across 641 districts. The implications are as urgent as they are sobering.
From Particles to People: The Pathways of Harm
At face value, “air quality” may sound abstract. But what the Health Benefit Assessment Dashboard (launched by Climate Trends and IIT Delhi) makes clear is that air quality is health writ small, human by human.
Here’s how the invisible becomes visceral:
PM₂.₅ refers to particulate matter smaller than 2.5 micrometers. Because of its minuscule size, it penetrates deep into the lungs, crosses into the bloodstream, triggers inflammation, oxidative stress, and disturbs multiple organ systems.
Over years of exposure, this process isn’t just local (lungs) — it can alter vascular function (raising blood pressure), impair insulin signaling (raising diabetes risk), disrupt red blood cell production (contributing to anemia), and affect fetal development (leading to low birth weight).
In children under 5, prolonged exposure damages respiratory defenses, heightens susceptibility to infections, and undermines iron status through inflammatory pathways.
Moreover, the effects are cumulative and compounding: early-life damage can predispose people to more severe disease trajectories later.
In short: long-term exposure to polluted air isn’t just a respiratory risk. It’s a multi-front assault on health.
What the Dashboard Tells Us: Numbers with Names
The real power of the dashboard lies in converting probabilities into human-scale impact. Drawing on district-level exposure and health survey data (NFHS-5), the tool simulates what might happen if PM₂.₅ were slashed by 30% across India — a target aligned with National Clean Air Programme (NCAP) ambitions.
Here are some headline projections:
For Women (ages 15–49)
Diabetes prevalence could decline from ~1.7% down to ~1.4% — a reduction in the burden of metabolic disease.
Hypertension risk could fall by 2% to 8%, depending on the state.
Cases of chronic obstructive pulmonary disease (COPD) may fall by 3% to 12%, especially in high-pollution states like Delhi, UP, Haryana.
Anaemia — often overlooked as an air-pollution outcome — could also see reductions.
These numbers may seem modest in percentage terms, but when multiplied across tens of millions of women, they represent enormous health dividends.
For Children (Under 5 Years)
Lower respiratory infections (LRIs): Cleaner air could reduce incidence significantly in high-risk districts (especially in the Indo-Gangetic plain).
Low birth weight (LBW): The chances of babies being born underweight could drop, particularly in states like Bihar, UP, Assam, Punjab, West Bengal.
Anemia in children: Less systemic inflammation and better iron metabolism could lead to improvements in anemia prevalence.
Importantly, the dashboard doesn’t treat India as a monolith. The geography matters: the highest gains are projected in the worst-polluted, most densely populated regions — exactly where vulnerability is greatest.
In some states, disease prevalence reductions approach one third. The dashboard authors even analogize it as “making the invisible visible” — turning air pollution into a public health narrative rather than an environmental abstraction.
The Human Toll: Voices Behind the Data
Numbers can quantify, but stories resonate.
Consider a pregnant mother in Patna inhaling auto emissions and coal dust for nine months — the stress, the oxidative damage, the silent restriction of oxygen and nutrient flow to her unborn child. The dashboard’s LBW projections become a personal tragedy avoided, a life trajectory altered.
Think of a toddler in Delhi, living in an inner-city slum, chasing after dust-laden winds. Each cough, each wheeze, is a micro-battle. The dashboard’s LRI statistics are not abstractions — they map to hospitalizations, days lost, fragile immune systems.
And women across states like Haryana, Punjab, Bihar may never synch their hypertension, diabetes, or anemia to “bad air.” But the dashboard says: look closer. The ambient air you breathe interacts with your body’s metabolism, oxidants, and inflammatory circuits.
Behind the dashboards are mothers, children, elders whose health is robbed slowly—sometimes invisibly—by particles in the air. The question is: will we allow that to continue?
Strengths, Innovations, and Caveats
Your project rests on several pillars of methodological innovation — and some inherent challenges:
What Makes It Strong
Granularity and scale: The district-level approach (641 districts) allows spatial resolution and helps policymakers zoom into hotspots.
Linking exposure to multiple outcomes: The dashboard integrates noncommunicable (e.g. diabetes, hypertension) and communicable / developmental (e.g. LBW, LRI, anemia) outcomes, painting a fuller picture.
Counterfactual scenario modeling: The “30% reduction scenario” anchors ambitions to realistic (though bold) air quality goals.
Public-facing dashboard: Turning modeling into a visual, interactive tool helps translate research into policy dialogue.
Points of Uncertainty / Limitations
Causality vs association: While epidemiological evidence supports strong links, modeling can’t fully remove residual confounding or reverse causation.
Uniform reduction assumption: The scenario assumes a uniform 30% cut in PM₂.₅ across diverse geographies — in reality, some districts might find it easier than others.
Exposure assignment error: Satellite-derived PM₂.₅ interpolations, assumptions about indoor / outdoor mix, and mobility of individuals can introduce exposure misclassification.
Nonlinear and threshold effects: Health impacts may not scale linearly with concentration changes; some benefits may accrue disproportionately at lower ranges.
Interaction with socioeconomic and behavioral variables: Nutrition, healthcare access, indoor pollution, smoking, and other co-factors may mediate or moderate the associations.
Despite these caveats, the dashboard is a powerful heuristic — a tool to shift thinking and spark action.
Policy Implications: Moving From Data to Justice
If air quality is health, then air policy is health policy. Here are vectors of urgency:
Align air quality targets with public health metrics. NCAP and state-level clean air plans should explicitly adopt health outcomes (e.g. reductions in hypertension, LRI) as metrics — not just “µg/m³”.
Target the worst offenders. States and districts projected to yield largest health gains should be prioritized (e.g. parts of UP, Bihar, Delhi, Haryana).
Sectoral interventions with health lens. Because different sources (transport, industry, domestic, biomass burning) contribute differently, targeting the most toxic species and sectors (as some component-level research suggests) can maximize gains.
Complement with health and nutrition programs. Cleaner air amplifies benefits of maternal-child health, iron supplementation, vaccinations, neonatal care.
Community awareness and empowerment. If women, mothers, local health workers understand that “bad air = more anemia or LBW risk,” they can demand cleaner neighborhoods, stricter enforcement, behavioral mitigation (e.g. air filtration).
Monitoring, evaluation, iteration. The dashboard itself can evolve — integrate newer survey rounds, refine exposure models, and track progress over time.
The goal: shift air quality from being treated as an environmental afterthought to a core pillar of public health strategy.
Into the Future: Breathing Hope
Imagine ten years from now: districts once choked by dust and smog record measurable drops in hypertension among women. Neonatal wards see fewer underweight infants. Rural communities, once burdened by childhood pneumonia, begin to register fewer cases. Lives extend, health improves — thanks not only to hospitals and medicine, but to cleaner skies.
This is not a utopian dream. The dashboard shows that with a “mere” 30% cut in PM₂.₅ — a feasible ambition — much of this is within reach for India.
But it requires a shift: from treating air pollution as a nuisance or a climate adjunct, to seeing it as a core determinant of health inequality. From fragmented policy to integrated health-environment strategy. From invisible harms to visible accountability.
Your work — making the invisible visible — is precisely the kind of bridge needed to jolt policy, public will, and scientific discourse. Let the data breathe life into change.




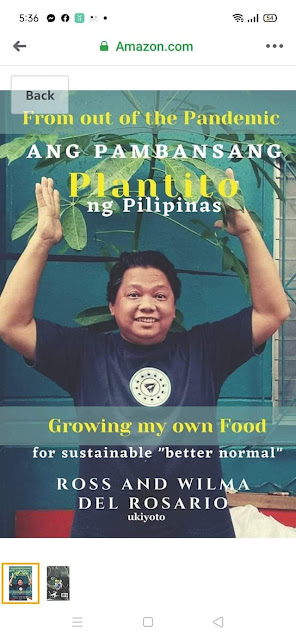
















 Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.
Ross is known as the Pambansang Blogger ng Pilipinas - An Information and Communication Technology (ICT) Professional by profession and a Social Media Evangelist by heart.






.jpg)





Post a Comment